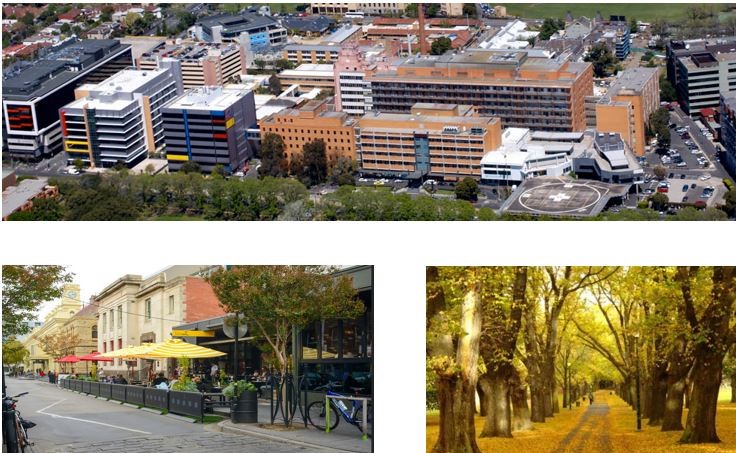
Austin Hospital
Austin Health – Upper Gastrointestinal and Bariatric Surgery Unit
Overview
The Upper Gastrointestinal and Bariatric Surgery Unit is part of the Division of General Surgery at Austin Health, a quaternary referral centre across two campuses, co-located with the University of Melbourne, Department of Surgery. The unit comprises 9 surgeons (all AANZGOSA members), including 3 university surgeons, who work across 2 campuses – Austin Hospital and the nearby Heidelberg Repatriation Centre. Oesophago-gastric, bariatric and general surgery as well as endoscopies are undertaken across both campuses. The oesophago-gastric and bariatric surgery fellows operate electively across these two campuses. Whilst emergency on-call work is undertaken at Austin Hospital.
Members of the Unit
9 consultant surgeons
– A/Prof Ahmad Aly (Head of Unit)
– Dr Tom Sweeney (Deputy Head)
– Dr Kiron Bhatia
– Dr Kiat Lim
– Dr Chek Tog
– Dr Krinal Mori
– Dr Ben Keong
– Dr Alex Craven
– Dr David Liu
2 Senior nurse coordinators: Ms Jarryd Walkley, Ms Linda Watson
1 Research nurse: Ms Amanda Dalyell
1 Oesophago-Gastric Surgery Fellow
1 Bariatric Surgery Fellow
2 General Surgery Registrar (SET trainee)
3 Interns
Key clinical activities
The Unit is one of the busiest oesophago-gastric and bariatric surgery units in the state. Per month there are:
– 28 public operating sessions
– 8 endoscopy list
– 4 Upper GI/General Surgery outpatient clinics
– 4 Bariatric Surgery outpatient clinics
– 2 Upper GI Cancer MDT meetings
– 1 Upper GI Benign disorder MDT meeting
– 1 Bariatric Surgery MDT meeting
– 4 Radiology meetings
– 4 Grand rounds
– Additional learning and teaching are undertaken during private operating lists
Elective operative experience/Case mix
– Oesophago-gastric resection (thoracoscopic, laparoscopic, open, and transgastric laparoendoscopic)
– Antireflux surgery and hiatus hernia repair
– Achalasia surgery (Heller’s myotomy and Peroral Endoscopic myotomy)
– Bariatric surgery (sleeve gastrectomy, gastric bypass, band removals, revisional surgery)
– Diagnostic and interventional endoscopy (POEM, dilatation, stenting, BOTOX injection, endoscopic mucosal resection, enteric access, foreign body retrieval, clipping, drainage, argon, laser, HALO, endoscopic management of bariatric complications)
– Abdominal wall reconstruction for complex hernias
– Cholecystectomy with trans-cystic choledochoscopy
– Elective General Surgery
– Both fellows participate in all public operating list at Austin and Repatriation Hospitals
– Fellows can expect 150-200 major Upper GI and bariatric cases per year, with more than 50% as the principal operator
– The Fellow will also access some work undertaken by consultant staff in various private hospitals including experience with the Da Vinci Robotic system
Emergency commitments
– Emergency General Surgery on-call: 1 in 4 rosters with the other General Surgery Units
– The Fellow takes second call, supporting a general surgical trainee on the on-call roster
Outpatient Experience
– 4 Upper GI and General Surgery clinics per month
– 4 Bariatric Surgery clinics per month
– Clinics are attended by consultants, fellows and registrars
– These sessions provide opportunities for assessment and management of individuals with UGI cancers, motility disorders, obesity, metabolic syndrome, and general surgery related pathologies
– The Unit views clinics as opportunities for teaching, discussion and cross-pollination of ideas
Perioperative Evaluation
– Preadmission and pre-op anaesthetic assessment clinics are coordinated by our senior nurse coordinators Ms Jarryd Walkley and Ms Linda Watson
– These clinics are attended by the Unit’s interns and the anaesthetic team, and is supported by the Unit’s Fellows
Prehabilitation and enhance recovery for UGI cancer and Bariatric Surgery
– Our unit is developing enhanced prehabilitation and recovery programs for UGI cancers and bariatric surgery
– The oesophago-gastric fellow will play a key role in facilitating these programs for UGI cancer surgery
– The bariatric fellow will play a key role in facilitating these programs for bariatric surgery
Multidisciplinary Interactions
There are regular clinical meetings involving interaction with multidisciplinary specialists. These include:
– Weekly radiology meetings
– Fortnightly UGI cancer multidisciplinary team meeting
– Monthly bariatric surgery multidisciplinary team meeting
– Monthly UGI benign disorder multidisciplinary team meeting
– The Unit views these meetings as highly educational, and all Fellows are expected to facilitate, attend, and contribute to these meetings
Education and Audits
In addition to clinical meetings, there are:
– Monthly Unit research meetings
– Weekly Surgical Forum hosted by the Division of Surgery, Anaesthesia and Procedural Medicine
– Weekly Austin Health Department of Surgery and Therapeutic Interventions audits
– Monthly Austin Precinct, University of Melbourne Department of Surgery Research meetings
– Monthly DOSTalks hosted by The University of Melbourne Department of Surgery
– Annual Unit audit
The Unit’s fellows are also expected to participate in teaching SET registrars on a formal basis. This includes:
– ‘Shock and Awe’ pre-fellowship exam tutorials
– Austin Surgical Education Program
– Annual UGI Surgery Saturday Surgical Seminar
The Fellows are provided with a workstation, computer, internet and printer access within the Clinical Surgical Unit. Fellows have full access to the onsite Austin Health Medical library which provides an extensive electronic literature database access.
Funding
The position is funded by the Austin Hospital. This is a form of a fixed annual salary covering both elective and emergent work. Additional income is generated from conjoint cases in private institutions. This will be on a regular schedule
Research Program
Most consultants within the Upper Gastrointestinal and Bariatric Surgery Unit have higher research degrees and ongoing interests in clinical research. The Unit is also intimately affiliated with the General and Gastrointestinal Surgery (GEGIS) Research Group embedded within the University of Melbourne Department of Surgery. Research from the Unit is regularly published in the field of Oesophago-Gastric and General Surgery. Undertaking research/audit project(s) is highly encouraged. The Fellows are expected to be involved in and submit for publication 1 or more manuscripts during his/her 12 month appointment.
Further information contact
A/Prof Ahmad Aly
aaly@outlook.com.au




 Introduction
Introduction